The visual inspection of a suspicious skin lesion using the naked eye alone is not enough to ensure the accurate diagnosis of skin cancer, a group of experts have concluded following a largescale systematic review of research.
The review is published today (Dec 6th) in The Cochrane Libraryas part of a Special Collection of Cochrane Systematic Reviews bringing together a large body of research on the accuracy of tests used to diagnose skin cancer. The suite of eleven reviews was led by Dr Jac Dinnes at the University of Birmingham and supported by the Cochrane Skin Group and a team of over 30 researchers and expert advisors. The work was funded by the National Institute for Health Research (NIHR).
The reviews summarise research evidence assessing the accuracy of different diagnostic tests to support clinical and policy related decision making in the diagnosis of all types of skin cancer.
Dr Jac Dinnes, of the University of Birmingham’s Institute of Applied Health Research, said: “Early and accurate detection of all skin cancer types is essential to manage the disease and to improve survival rates in melanoma, especially given the rate of skin cancer world-wide is rising.
“The visual nature of skin cancer means that it can be detected and treated in many different ways and by a number of different types of specialists, therefore the aim of these reviews is to provide the world’s best evidence for how this endemic type of cancer should be identified and treated.
“We have found that careful consideration should be given of the technologies that could be used to make sure that skin cancers are not missed, at the same time ensuring that inappropriate referrals for specialist assessment and inappropriate excision of benign skin lesions are kept to a minimum.”
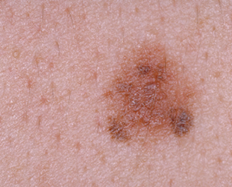
There are three main forms of skin cancer. Melanoma and cutaneous squamous cell carcinoma (cSCC), are high-risk skin cancers with the potential to spread and cause death.
A basal cell carcinoma (BCC) rarely spreads, usually remaining localised with potential to infiltrate and damage surrounding tissue.
Key findings of the Special Collection were:
- Visual inspection using the naked eye alone is not good enough and melanomas may be missed.
- Smartphone applications used by people with concerns about new or changing moles or other skin lesions have a high chance of missing melanomas.
- When used by specialists, dermoscopy — a technique using a handheld device to zoom in on a mole and the underlying skin — is better at diagnosing melanoma than visual inspection alone, and may also help in the diagnosis of BCCs.
- Dermoscopy might also help GPs to correctly identify people with suspicious lesions who need to be seen by a specialist.
- Dermoscopy is already widely used by dermatologists to diagnose melanoma but its use in primary care has not been widely evaluated therefore more specific research is needed.
- Checklists to help interpret dermoscopy might improve the accuracy of diagnosis for practitioners with less expertise and training.
- Teledermatology — remote specialist assessment of skin lesions using dermoscopic images and photographs — is likely to be a good way of helping GPs to decide which skin lesions need to be seen by a skin specialist but future research needs to be better designed.
- Artificial intelligence techniques, such as computer-assisted diagnosis (CAD), can identify more melanomas than doctors using dermoscopy images. However, CAD systems also produce far more false positive diagnoses than dermoscopy and could lead to considerable increases in unnecessary surgery.
- Further research is needed on the use of specialist tests such as reflectance confocal microscopy (RCM) — a non-invasive imaging technique, which allows a clinician to do a ‘virtual biopsy’ of the skin and obtain diagnostic clues while minimising unnecessary skin biopsies. RCM is not currently widely used in the UK but the evidence suggests that RCM may be better than dermoscopy for the diagnosis of melanoma in lesions that are difficult to diagnose.
- Other tests such as using high frequency ultrasound have some promise, particularly for the diagnosis of BCCs, but the evidence base is small and more work is needed.
Cochrane Skin Group founder Professor Hywel Williams, of the Centre of Evidence-Based Dermatology at the University of Nottingham, said: “Completing this broad suite of detailed reviews was a real marathon.
“Apart from a few exceptions, I was surprised by how poor the overall study designs were, especially in terms of accurately documenting where on the clinical pathway patients were tested.
“Although some useful conclusions have emerged, for example, on the role of dermoscopy, the greatest value of the research is to serve as a yardstick for designing future studies evaluating skin cancer diagnosis techniques on patients who are typically seen in GP and specialist settings.”
The research team said that future studies evaluating diagnostic skin cancer tests should recruit patients with suspicious skin lesions at the point on the clinical pathway where the test under evaluation will be used in practice.
Further research is also needed to evaluate whether checklists to assist diagnosis by visual inspection alone can improve accuracy and to identify how much accuracy varies according to the level of expertise of the clinician carrying out the assessment.
Well-designed studies of dermoscopy in primary care are needed, and the best ways of delivering dermoscopy training need to be identified.
The reviews have been shared with The National Institute for Health and Care Excellence (NICE) to inform a potential update of the NICE Melanoma guideline, which was last updated in 2015.